The Birth Of Phototherapy
Jaundice, also known as icterus, is a term used to describe a yellowish tinge to the skin and sclerae (the white part of the eye) that is caused by an excess of
 bilirubin in the blood (hyperbilirubinaemia).
bilirubin in the blood (hyperbilirubinaemia).
Up to 80% of normal newborn babies become clinically jaundiced sometime during the first week of life. For the majority of cases, there will be no pathological effects, but these babies do need to be monitored because bilirubin is potentially toxic to the central nervous system.
The use of phototherapy is an established and widely used treatment for newborn babies with severe jaundice; but how does it work?
Biochemistry of jaundice
Bilirubin is a normal breakdown product of red blood cells (it is derived from haem). Free bilirubin is toxic and must be transformed (conjugated) by the liver so it can be removed from the body.
A normal healthy full-term baby may be jaundiced from days 2-8, and for premature babies, jaundice may be present from days 2-14. This ‘physiological’ jaundice is extremely common and often does not require treatment; however if bilirubin concentrations are very high then treatment may be necessary. ‘Physiological jaundice’ results in an unconjugated hyperbilirubinaemia and is usually caused by liver immaturity, or may sometimes be seen in babies who are exclusively breast fed.
Any jaundice appearing at <1 day of age or persisting after 14 days is likely to be pathological. Pathological hyperbilirubinaemia may be caused by a number of conditions, such as haemolytic disorders, congenital hypothyroidism and some inherited metabolic diseases.
What is phototherapy?
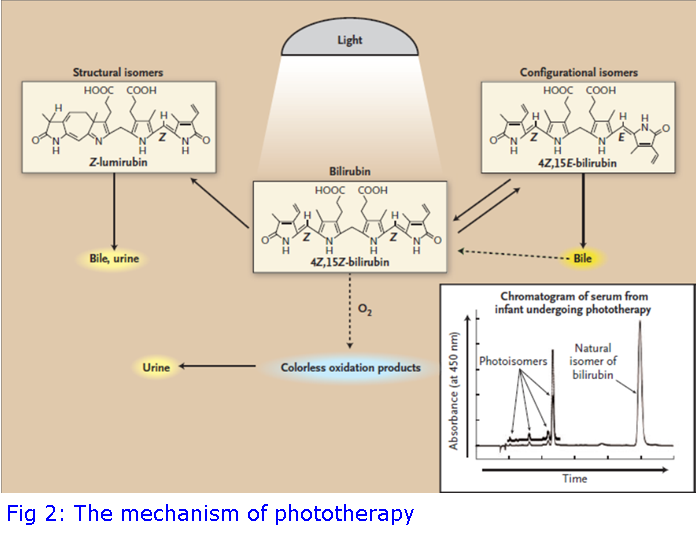
Phototherapy uses blue light to change the shape and structure of bilirubin to forms that can be excreted. It is a common misconception that UV light is used for phototherapy, but it is not: Blue light, at a wavelength of 460-490 nm, is directed onto the baby’s skin where it is absorbed to convert bilirubin to photoisomers and oxidation products for excretion. There are several forms of phototherapy available and depending on the severity, this may be a glowing blanket that parents can wrap around their baby at home, or a crib with multiple lights used in the hospital.
History of phototherapy
The effect of light on jaundice in newborns was first discovered in the 1950s at Rochford General Hospital, Essex, with a little bit of science and a lot of luck!
Sister J Ward was in charge of the Premature Baby Unit at the hospital and believed in the benefits of fresh air and warm sunshine over the confines of a stuffy incubator. She would take babies outside on warm summer days, bringing them in quickly before the consultants were doing their ward round. During one of these rounds, a Dr Dobbs noticed a triangular patch of skin on one of the jaundiced babies which was much more yellow than the surrounding skin. Dr Dobbs asked about this, to which Sister Ward replied she thought it might be an effect of the sun. Upon further interrogation, she confessed that she’d been taking the babies outside, and it was actually that the baby was less yellow than before: the triangular patch was where the sheet had covered the baby. This observation was not followed up; the baby got better and was discharged home.

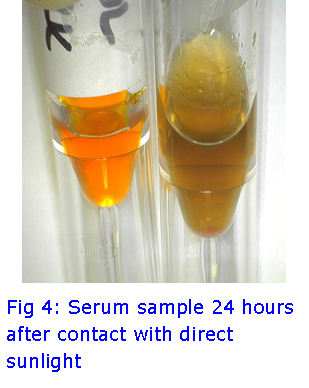
On a sunny day a few weeks later, blood was sent to the laboratory for another jaundiced baby. The serum was analysed for bilirubin and the result reported was much lower than expected, and did not fit with previous analyses. The biochemist in the laboratory, Mr Perryman, apologised to Dr Dobbs saying that the sample had unfortunately been left on the windowsill and forgotten about. Mr Perryman had re-measured the bilirubin and it was even lower than before. Mr Perryman also noticed the serum sample was no longer the yellow colour associated with jaundice, but had gone green.
The penny dropped... Light seemed to affect bilirubin... Further work was undertaken and it was soon established that blue light seemed to affect bilirubin concentrations; the light only affected unconjugated bilirubin and the green colour was due to the presence of biliverdin, a conversion product of bilirubin thought to be harmless to brain cells. Back in the Premature Baby Unit, jaundiced babies were cautiously allowed outside for exposure to sunlight, and their jaundice disappeared faster than if they were left inside the ward.
Recreating the history
The Blood Sciences Laboratory at Viapath was recently approached by the BBC and asked if it would be possible to recreate Mr Perryman’s discovery. Serum from jaundiced babies was collected and taped to the window in direct sunlight. After only 24 hours in the sun, the bright yellow jaundiced serum had turned green, indicating the conversion of bilirubin to biliverdin. Bilirubin concentrations were also measured over the following days and it was shown that there was a significant decrease in the bilirubin concentration even at day 1.
Our work is scheduled to be broadcast on the BBC One Show in March 2017.
Viapath’s Services
In the Blood Sciences Laboratory at Viapath, we offer total bilirubin and conjugated bilirubin measurements to aid in the diagnosis of jaundice for children and adults.
Please contact the Blood Sciences Laboratory at St. Thomas’ for further information on bilirubin analysis on 0207 188 9247 or by email:
Dr Sally Brady, Consultant Clinical Scientist: sally [dot] brady [at] viapath [dot] co [dot] uk
Steve Wilkins, Operations Manager, stephen [dot] wilkins [at] viapath [dot] co [dot] uk
Darren Costello, Service Delivery Manager: darren [dot] costello [at] viapath [dot] co [dot] uk
References
Cremer RJ, Perryman PW & Richards DH, 1958. Influence of light on the hyperbilirubinaemia of infants. Lancet 1(7030), 1094-1097.
Dobbs RH & Kremer RJ, 1975. Phototherapy. Archives of Disease in Childhood 50, 833-836.
Maisels MJ & McDonagh AF, 2008. Phototherapy for neonatal jaundice. NEJM 358(9), 920-928.