Platelet Research Project Impacts Clinical Practice Of Top Cosmetic Dentist To Directly Improve Patient Care.
Platelets are circulating, anucleate cytoplasmic fragments of their parent cells, the megakaryocytes, which are confined to the blood cell manufacturing compartments inside bones. Each megakaryocyte produces between 2000 – 3000 platelets which are then released into the bloodstream. Whilst platelets tend to be considered as having their primary role in haemostasis, the process of blood clotting, they are intricately involved in the initiation of wound healing. Indeed, haemostasis can be considered as the first stage of blood vessel healing. Despite being mere cell fragments, platelets have complex, specialised structure and physiology in order fulfil their dual role.
A number of specialised structures are present in platelet cytoplasm, the most abundant of which are the α-granules. These granules contain an array of molecules essential to both haemostasis and wound healing. Platelets activated by the clotting process release α-granule contents into the immediate vicinity of the wound and the clot to concentrate vital molecules for haemostasis and wound healing. Some of the molecules are termed growth factors as they promote healing processes, and others, such as fibronectin directly take part in tissue repair.
How can we harness the wound healing properties of platelets in the clinical setting?
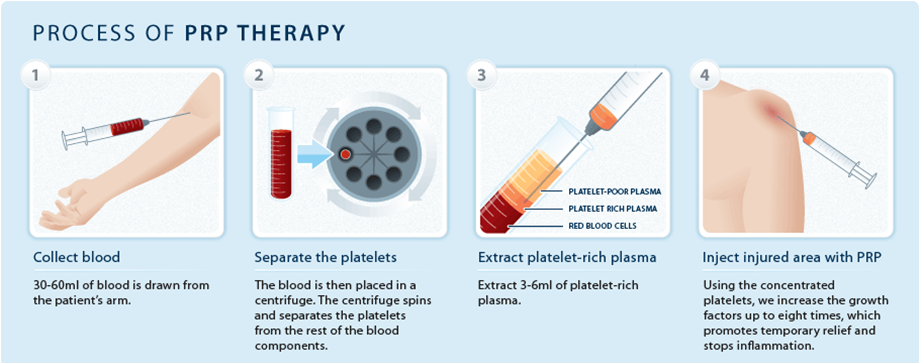
It is possible to concentrate platelets from patient blood samples by removing the red and white blood cells, leaving behind the platelets suspended in the fluid that transports the cells along blood vessels, the plasma. This is termed platelet-rich plasma (PRP) and recent years have seen an increase in the use of applying the patient’s own PRP to wounds to promote soft and hard tissue regeneration and speed up healing. Using the patient’s own cells means rejection is not a problem, it is cheaper and safer than artificial growth factors, and matches natural healing mechanisms. Patient’s PRP has been used in treatment of chronic skin and soft tissue ulcers and many surgical and dental settings. The PRP can be activated to ensure growth factor release.
How can Viapath help?
Platelets have a short lifespan of 8-10 days in the body and are viable for only 5 days when stored for transfusion purposes. There are few data on PRP stability when stored for promoting tissue repair and patients often have blood taken daily to generate fresh PRP. The Haemostasis & Thrombosis Laboratories at St. Thomas’ Hospital were recently approached by one of the UK’s pioneers in use of PRP in dentistry, Dr Mitra Najafi of Stardent, to investigate platelet and growth factor stability in stored PRP to ascertain whether she could reduce the frequency of bleeding her patients.
What did we do?
Dr Gary Moore, Consultant Scientist for Haemostasis & Thrombosis, designed a study that stored (his own) PRP under a variety of conditions. The platelets were tested daily for platelet numbers and structural integrity, functional responses to activation, and the amount of growth factor released during activation. The functional testing involved activating the PRP with collagen because that is what Dr Najafi employs in her clinical practice.
The expertise of numerous colleagues was needed to complete the project, with Robert Archer and Kerri Brown testing platelet integrity and function, and James Maloney, Kasia Mayger and Elaine Bromidge working on a new assay to measure the released growth factor.
The testing was done over an eight day period and showed that although platelets deteriorate over time, as was anticipated, they retain significant growth factor availability for up to 5 days when stored in a particular type of container at room temperature, and intermittently mixed to reduce spontaneous aggregation (platelets sticking to each other).
Clinical outcomes
A detailed report was submitted to Dr Najafi who was then able to alter her clinical practice and reduce frequency of bleeding and PRP generation based on objective evidence. As well as dentistry, Dr Najafi uses PRP in a non-surgical anti-ageing procedure called the Vampire Facelift because it first involves taking the blood from the patient and removing the red and white cells before undertaking multiple injections (vampire bites!) of the PRP into the skin of the face to promote tissue repair and rejuvenation. It is also more palatably referred to as the Natural Facelift as the platelet-derived growth factors regenerate tissue by recruiting the patient’s own stem cells.
Scientific achievements
The Diagnostic Haemostasis & Thrombosis Laboratory team were able to combine Viapath’s core professional values of innovation, collaboration and expertise to design and deliver a project of sufficient rigour to inform clinical practice of a service user. The study was considered sufficiently useful to the wider scientific and clinical communities to warrant submission to an international, peer reviewed journal and was published in October 2016 with the following citation:
Moore GW, Maloney JC, Archer RA, Brown KL, Mayger K, Bromidge ES, Najafi MF. Platelet rich plasma for tissue regeneration can be stored at room temperature for at least five days. British Journal of Biomedical Science 2016 Oct8: 1-7. [Epub ahead of print].
For more information on the study, details about the department’s platelet diagnostics or to receive a copy of the paper, please contact:
Dr Gary Moore
Consultant Biomedical Scientist, Diagnostic Haemostasis and Thrombosis Laboratories, St. Thomas’ Hospital
Telephone: 020 7188 0814
Email: gary [dot] moore [at] viapath [dot] co [dot] uk
Other publications relating to platelets:
Posters:
Gurney DA, Moore GW, Rangarajan S. Platelet glycoproteins: predictors or progression markers in cardiovascular disease? International Society on Haemostasis & Thrombosis 2007, Geneva.
Mitchell MJ, McCormick Á, Maloney JC, Moore GW, Austin SK. A reduced response to TRAP-6 in platelet aggregometry studies is not usually due to a PAR-1 receptor defect. International Society on Haemostasis & Thrombosis 2015, Toronto
Publications:
Okoli S, Madan B, Mwirigi A, Moore GW, Drew A, Mitchell MJ, Cutler JA. A diagnostic dilemma: Variant Bernard-Soulier syndrome, a difficult clinical and genetic diagnosis. Haemophilia. 2015;21:e479-e525
Moore GW. Normal Haemostasis. In: Moore GW, Knight G, Blann AD. Fundamentals of Biomedical Science. Haematology. Oxford University Press, UK: First edition 2010; Second edition 2016
Moore GW & Gurney DA. Bleeding Disorders and their Laboratory Investigation. In: Moore GW, Knight G, Blann AD. Fundamentals of Biomedical Science. Haematology. Oxford University Press, UK: First edition 2010; Second edition 2016

