Early experience with the interpretation of dp-ucMGP: an indicator of vascular calcification
FOCUS 2018, the national meeting of the Association for Clinical Biochemistry and Laboratory Medicine, covered various topics on laboratory medicine and provided an opportunity for an enhanced, constructive dialogue on Viapath’s new diagnostic test - Matrix Gla Protein (MGP).
The role of Matrix Gla Protein
Matrix Gla Protein (MGP) is a 84 amino acid extra hepatic vitamin K-dependent protein which is synthesized by chondrocytes and vascular smooth muscle cells. It plays an essential role in the regulation of bone and soft tissue calcification by directly inhibiting calcium precipitation and crystallization, and is the most potent inhibitor and reverser of arterial calcification currently known. Knock-out mice lacking MGP develop extensive and premature calcification in arteries and cartilages and die within six to eight weeks of birth as a result of blood-vessel rupture.
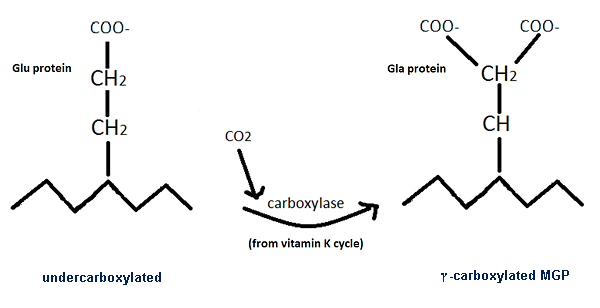
MGP activation is expressed through two posttranslational processes: the phosphorylation of three serine residues in positions 3, 6, and 9 (although the role of this phosphorylation process is still not well understood) and the carboxylation of five glutamate residues. For this reason, different forms of MGP are circulating in plasma which may have different physiological roles and functions. Studies on the different species of MGP have shown that the dephosphorylated and uncarboxylated (dp-ucMGP) form is the only variant associated with a response to vitamin K supplementation. Increased levels of dp-ucMGP reflect an increased propensity for vascular calcification and decreased availability of vitamin K in the vessel wall. The measurement of dp-ucMGP has been suggested to be a functional indicator of vitamin K status in tissues that utilize MGP. Also, it is possible that the measurement of dp-ucMGP reflects vitamin K status.
Measurement of MGP
In a recent study, we measured the desphosphorylated-uncarboxylated form of MGP (dp-ucMGP) using an automated IDS-iSYS InaKtif MGP assay based on chemiluminescent technology to begin to evaluate the clinical utility of this marker in patients with established vascular risk factors..
35 plasma samples were analysed from patients with: type 2 diabetes mellitus (T2DM), (n=4); chronic kidney disease (CKD), (n=4); rheumatic disease (RD), (n=3); hypertension (HTN), (n=6); raised total cholesterol (>4mmol/L), (n=11); and cardiovascular disease (CVD) (n=6). In addition, 80 plasma samples were analysed from postmenopausal osteoporotic women aged ≥55 y who were receiving oral bisphosphonate treatment and had low serum vitamin K1 concentrations ranging from 0.05-0.35µg/L [fasting reference range; 0.17–0.68µg/L].
The MGP cut-off value <750pmol/L was adopted from manufacturer’s reference range. It was calculated from 132 apparently healthy donors from 18 to 59 years of age, using the IDS-iSYS InaKtif MGP assay.
The incidence of elevated dp-ucMGP was: 33% in CVD (mean 641pmol/L); 33% in RD (mean 725pmol/L); 33% in HTN (mean 674pmol/L); 25% in T2DM (mean 716pmol/L); and 18% in raised cholesterol (mean 610pmol/L). In the osteoporotic women, 9% had a dp-ucMGP that exceeded the cut-off value (mean 534pmol/L). In addition, in keeping with previous published studies (Riphagen 2017, Theuwissen 2014), we found a significant association between age (r=0.31, p < 0.05) and BMI (r=0.4, p=0.001) with dp-ucMGP. Both increasing age and BMI are associated with the risk of CVD and the correlation observed here may suggest that the link between obesity and CVD could be modulated by MGP but further research is needed.
Conclusion
Our results show more >750 pmol/L values in patients at high risk of CVD, and a positive correlation with age and BMI: both CVD risk factors. Both increasing age and BMI are associated with the risk of CVD and the correlation observed here may suggest that the link between obesity and CVD could be modulated by MGP but further research is needed. When the serum vitamin K1 levels were spilt into quartiles, there was no significant difference in dp-ucMGP concentrations. The vitamin K1 concentrations were below the reference range median; thus evaluation with a larger range is needed.
Studies have shown that vitamin K supplementation reduces dp-ucMGP and improves vascular health. Monitoring dp-ucMGP levels may allow modulation of arterial calcification and CVD progression, particularly in those with increased age and BMI.
For further information, please contact:
Human Nutristasis Laboratory: 0207188 6815 / 89543
Renata Gorska:
renata [dot] gorska [at] viapath [dot] co [dot] uk
Acknowledgement:
Marianne Bradley, Renata Gorska, Amelia Moore, Geeta Hampson and Dominic Harrington (The National Meeting in Manchester FOCUS 2018 – poster presentation)
References:
- Cranenburg EC1, Koos R, Schurgers LJ, Magdeleyns EJ, Schoonbrood TH, Landewé RB, Brandenburg VM, Bekers O, Vermeer C. Characterisation and potential diagnostic value of circulating matrix Gla protein (MGP) species. Thrombosis and haemostasis. 2010, 104. 811-22.
- Luo G, Ducy P, McKee MD et al. Spontaneous calcification of arteries and cartilage in mice lacking matrix GLA protein. Nature 1997 Mar 6;386(6620):78-81
- Riphagen, I.J.; Keyzer, C.A.; Drummen, N.E.A.; de Borst, M.H.; Beulens, J.W.J.; Gansevoort, R.T.; Geleijnse,3. J.M.; Muskiet, F.A.J.; Navis, G.; Visser, S.T.; Vermeer, C.; Kema, I.P.; Bakker, S.J.L. Prevalence and Effects of Functional Vitamin K Insufficiency: The PREVEND Study. Nutrients 2017, 9, 1334.

