Breathing New Life Into The Diagnosis Of Respiratory Infections
Since December 2015 there have been significant advances in the way Viapath’s Infection Sciences Laboratory at St. Thomas’ Hospitaltests for respiratory tract infections. The development work that enabled these advances was partially funded by a grant from Guy’s and St. Thomas’ Charity.
What is the burden of respiratory tract infections?
Respiratory tract infections are an important cause of morbidity and mortality, particularly affecting the very young, the elderly and those with underlying health conditions. These infections not only place pressure on the NHS but also contribute to the loss of many working days and the knock-on financial and social impact on society as a whole.
During the winter months hospital admissions due to influenza place a significant pressure on availability of hospital beds and this has been highly publicised in the mainstream media in recent years. Public Health England figures for winter 2015-16 state that there were 2462 Intensive Care Unit (ICU) admissions due to influenza infections, resulting in 209 deaths1. Timely diagnosis of influenza is important both for infection control and for implementing treatment and prophylaxis with antiviral agents.
Community acquired pneumonia (CAP) also peaks in the winter, although it does occur all year round. The incidence of CAP is approximately 5-11 cases per 100 000 population, with about one fifth needing hospital admission. About 5-10% of these patients need intensive care and half of those will die. In approximately half of all pneumonia cases, the causative pathogen is not identified due to limitations of some diagnostic methods. For example, some pathogens do not grow well or at all on standard microbiological media, serological diagnosis is too slow and can be inaccurate, and historically molecular tests had slow turnaround times due to referral to external specialist laboratories. Provision of molecular testing locally would significantly improve both accuracy and timeliness of diagnosis in these cases.
What are the new tests?
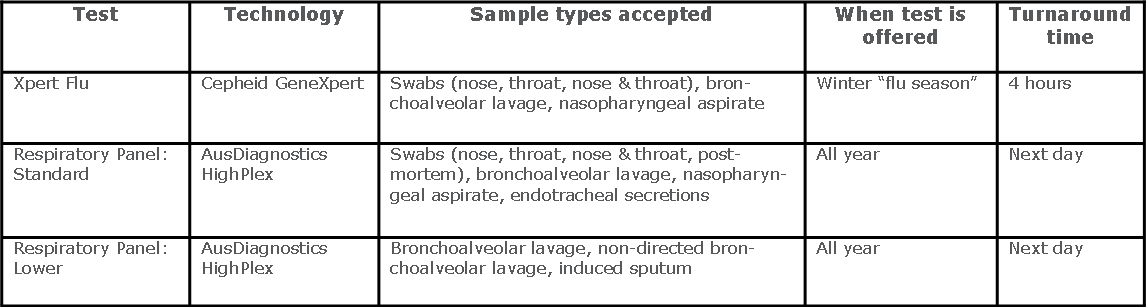
AusDiagnostics HighPlex technology for the “Respiratory Virus Panel” was introduced by Viapath’s Virology laboratory in December 2015 for simultaneous detection of nine different respiratory viruses. One year later an additional assay was introduced using the same technology but for the detection of seven non-viral pathogens in the lower respiratory tract of severely ill patients, including Legionella pneumophila, Mycoplasma pneumoniae, Chlamydophila psittaci and Pneumocystis jiroveci.
December 2016 also saw Viapath’s Microbiology laboratory introduce a rapid molecular influenza and respiratory syncytial virus (RSV) test, using Cepheid’s GeneXpert sample-to-answer technology. This platform enabled the provision of a 24/7 service producing results within 2 hours of the sample being received in the laboratory.
There will be a further update in respiratory virus testing in April 2017, with the introduction of a new panel which includes M. pneumoniae and Bordetella pertussis (the causative agent of whooping cough) plus eight respiratory viruses on the AusDiagnostics platform. Samples from both the upper and lower respiratory tract can be tested using this assay, making it a particular improvement for the timely diagnosis of B. pertussis and M. pneumoniae infections.
How have these assays improved diagnosis? What is the clinical impact?
Introduction of these three new assays has increased the number of important respiratory pathogens that can now be rapidly detected from routine clinical specimens in our own laboratory. Local provision of molecular assays for detection of pathogens causing non-viral respiratory infections and the introduction of the GeneXpert platform for urgent influenza testing has significantly improved turnaround times for these assays. The clinical benefit of these new assays includes the ability to stop unnecessary use of antibiotics earlier, better targeting of therapy for unusual infections, better use of limited isolation facilities and potentially better outcomes for patients. It is also helpful to provide a definitive diagnosis early so that clinicians don’t spend time and resources performing additional diagnostic tests. This is particularly beneficial for patients in the Severe Respiratory Failure Centre in the Intensive Care Unit, as ICU Consultant Nick Barrett explains: “Within the severe respiratory failure population in intensive care, especially those requiring Extra-Corporeal Membrane Oxygenation (ECMO), history and examination are virtually useless in providing clear direction for diagnosis. Hence we rely on a broad brush of rapid, accurate diagnostics in order to provide the optimal therapy to the patient as rapidly as possible. For this population, access to rapid PCR tests for viruses, typical bacterial and atypical pathogens is essential to give the right therapy at the right time. The right diagnosis allows early escalation/de-escalation of antimicrobials and the appropriate use of personal protective equipment and isolation facilities, the latter being a relatively scarce resource. Rapid diagnostics being in routine use improves the care for our patients and better application of resources.”
For further information contact
Penny Cliff, Clinical Scientist, Infection Sciences
Email: penny [dot] cliff [at] viapath [dot] co [dot] uk (subject: pathology%40viapath)
Emma Cunningham, Clinical Scientist, Infection Sciences
Email: emma [dot] cunningham [at] viapath [dot] co [dot] uk (subject: pathology%40viapath)
References
- Public Health England (2016). Surveillance of influenza and other respiratory viruses in the United Kingdom: Winter 2015 to 2016.
- Cunningham, E., Cliff, P., O’Shea, S., MacMahon, E. (2016). Utility of the AusDiagnostics HighPlex Platform for Diagnosis of Respiratory Viruses and Atypical Pneumonia Pathogens. ECCMID ePoster EV0111.

