‘Dying for a tan’ - Evidence for photocarcinogenesis
The incidence of skin cancer is rising. It is the most common type of cancer in the U.S. In fact, the Skin Cancer Foundation estimates (http://www.skincancer.org/skin-cancer-information/skin-cancer-facts) that one in five Americans will develop some form of the disease in their lifetime. According to the Foundation’s web site, “nearly 800,000 Americans are living with a history of malignant melanoma (MM) and 13 million are living with a history of non-melanoma skin cancer, typically diagnosed as basal cell carcinoma (BCC) or squamous cell carcinoma (SCC)”. In the UK, around 102,000 cases of non-melanoma skin cancer are diagnosed each year. Cancer Research UK figures (2014) state that there were around 15,400 new cases of melanoma skin cancer in the UK. That’s 42 cases diagnosed every day. Melanoma skin cancer is the fifth most common cancer in the UK (2014) and it accounts for 4% of all new cases. In the case of non-melanoma skin cancer the stated figures are, in reality, a considerable under-estimate, as a percentage of BCC’s never get recorded as many people do not seek medical treatment for them.
The most significant risk factor for the development of both melanoma and non-melanoma skin cancer is exposure to the sun’s rays. It is within the spectrum of ultra violet light, most significantly UVB (wavelength 280-315nm) and to a lesser extent UVA (wavelength 315-400nm), that is commonly associated with photo induced sun damage to our skin.
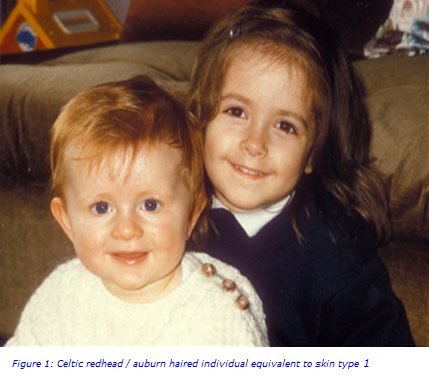
Broadly speaking there are 6 skin types (I-VI) in the world. Each skin type has differing tanning ability and also varying degrees of resistance to the development of skin cancer. Skin type I (the northern European or Celtic skin type) is the most susceptible to the development of skin cancer and correspondingly this skin type also has the least tanning ability. Conversely skin type VI (the Afro-Caribbean population) is the least susceptible to the development of skin cancer and has the highest tanning ability (Figures 1 and 2).

As we age there is a chronological deterioration in the healthy functioning of our skin. Significantly the more exposure we have to sunlight during our life time, the more rapid these degenerative changes are likely to be. The harmful effects of exposure to UVA and UVB include:
- Acute inflammation (sunburn/erythema)
- DNA and oxidative damage
- Mutation (e.g. p53)
- Immunosuppression
- Skin cancer
- Photoageing
- Photodermatoses (premalignant skin lesions such as solar keratosis and actinic keratosis)
A recently published large cohort study of 109 thousand women in the US, from the years 1989-2009, looked at the incidence of BCC, SCC and MM1. The study revealed that for MM, participants with 5 or more blistering sunburns between ages of 15-20 years old resulted in an 80% increase in the chances of developing MM, similarly there was also a 68% increase in the chances of developing BCC or SCC. Such data shows a close correlation with sunburn episodes and the likelihood of developing skin cancer later in life. Studies evaluating the significance of sunburn episodes in young life (before the age of 10) show a frighteningly similar, if not more elevated, trend analysis. In addition to the growing data on the risks associated with natural sunlight exposure, there is also a worrying trend with the associated risk related to the exposure to artificial sunlight in the form of sun bed usage. Across USA and Europe, 40-50% of teenagers between the ages of 15-18 years old, have used indoor tanning devices with the highest incidence recorded in Scandinavia and Minnesota2. Epidemiological studies have shown that exposure to sunbeds increases the risk of both melanoma and non-melanoma skin cancers. There is also an increased risk with long term usage (cumulative exposure). The associated risk of sunbed use in MM patients younger than 30 years old may be as high as 43-76% depending on which studies you read. The fundamental premise is that sun bed usage in adolescents should be strongly discouraged.
In terms of photobiology, the key sequences that result in carcinogenesis involve signal transduction pathways, oncogene and tumour suppressor gene interactions, DNA damage and repair processes, immunological surveillance and the significance of chemo-preventive and/or therapeutic agents. What is becoming increasingly apparent is the fact that cumulative ‘sun burn episodes’ do a great deal of harm to our skin over our life time and these effects are often non reversible. Thus studying the effects of ‘sun burn episodes’ has formed the basis of unravelling the long term effects of sun damaged skin changes. (Figure 3)
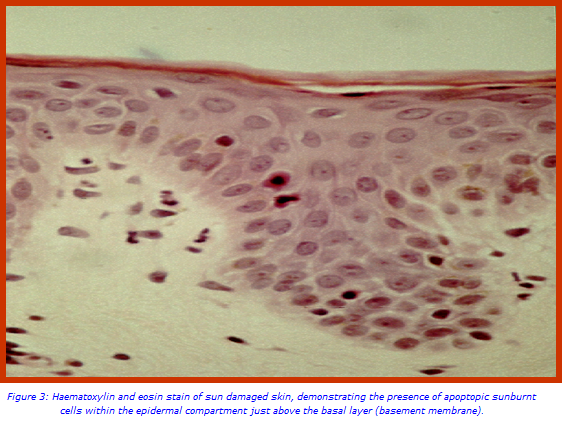
Histological evaluations of trials based on assessments of minimal erythemal dose (MED) sun burn episodes on skin, provide us with an insight into what cellular changes can be seen immediately following a sun burn episode and, then subsequently, how our skin undertakes repair processes that enable the skin to return back to a normal state. It also provides data on the consequences of repeated sun burn episodes. Evaluation of antibody panels to assess cellular changes in this manner include markers for cellular proliferation such as Ki67, Thymine Dimer markers for DNA damage, p53 for oncogene expression, CD1a for monitoring immune surveillance of Langerhan cells within the epidermal compartment and also apoptosis regulator makers such as Bcl2. These studies, if done in parallel with the same individuals whilst also examining sunscreen protected skin, can act as a good control to study the cause and effect of photodamage and photocarcinogenesis analysis. A fairly consistent observation in studies of this type reveals that p53 expression is depleted in sun screen protected sites and Langerhan cells actively migrate away from the epidermal compartment even when mild erythema (sun burn) is present. In conclusion the use of daily sunscreens can prevent the epidermal effects of repeated daily-erythemal solar simulating radiation (SSR) exposure.
The evidence indicates that sun tans are in fact contributing to the damage caused by the sun to skin in a long term manner.
Acknowledgment
This article reflects studies performed in collaboration with Professor Antony Young at St. John’s Photobiology Research Unit, St. John’s Institute of Dermatology, Kings College London.
For further information, please contact:
Dr Guy Orchard, Consultant Grade Biomedical Scientist/Laboratory Manager
Email: guy [dot] orchard [at] viapath [dot] co [dot] uk
References
- Long-term ultraviolet flux, other potential risk factors, and skin cancer risk: a cohort study. Wu.S, Han.j, Laden. F, Qureshi. A.A. Cancer Epidermiology Biomarkers and Prevention 2014: 23(6); 1080-9.
- Tanning salons and skin cancer. Dore JF, Chignol MC. Photochem Photobiol Sci. 2012 11(1): 30-7
- The detrimental effects of daily sub-erythemal exposure on human skin in vivo can be prevented by a daily-care broad-spectrum sunscreen. Young.AR, Orchard GE, Harrison GL, Klock JL. J. Invest. Dermatol. 2007. 127(4): 975-8.

